II Artificial Intelligence in Healthcare Symposium and Datathon
- Symposium
- Richard Delaney - Vital Strategies
- Nick Guldemond - The Institute of Health Policy & Management Erasmus University
- Jacson Venâncio Barros - President of the Brazilian Association of CIO’s in Health
- Round Table: Challenges of Big Data and AI in Population Health - Gisele Bohn, Richard Delaney, Nick Guldemond, Jacson Barros, Fatima Marinho
- Open Session: Data Access, Privacy and Security - Andrea Suman, Silvio Pereira, Anderson Soares, Marcelo Felix, Rogéria Leoni Cruz
- Leonardo Rolim Ferraz
- Lucas Bulgarelli - MIT/HIAE
- Ary Serpa Neto - HIAE
- Christopher Cosgriff - MIT
- Round Table: Challenges of Big Data and AI in the Intensive Care Unit - Leo Anthony Celi, Alistair Johnson, Leonardo Rolim Ferraz, Ary Serpa Neto, Lucas Bulgarelli
- Leo Anthony Celi - MIT
- Alistair Johnson - MIT
- Matthieu Komorowski - Imperial College London
- Open Session: Opportunities for Innovation in Healthcare - Pedro Marton Pereira, Gustavo Landsberg, Gisele Bohn, André Bem
- Datathon
From April 25-27th 2019 Hospital Israelita Albert Einstein (HIAE), the PROADI-SUS project and MIT organized its Artificial Intelligence in Healthcare Symposium and Datathon.
In the first day, we attended a Symposium including talks and round tables with experts in the field of Artificial Intelligence, Big Data and Healthcare. I took some notes of things I found interesting and will be posting here for further consultation.
Symposium
Richard Delaney - Vital Strategies
Intersection Between High-dimensionality Data and Established Public Health Databases
- High Dimensional Data:
- Many factors to control for, harder to do hypothesis testing. One alternative is to leverage machine learning to do more pattern recognition
- Don’t always come with pre conceived ideas, but try to find patterns freely
- Find probabilities of actions to know where to deliver Public health service
- Creating conditions to success:
- Start with a project: avoid “We prepare and then we act”, we are never prepared enough! Start easy, purposeful, datathon events follow this idea!
- After the first step, discuss systemic changes
Nick Guldemond - The Institute of Health Policy & Management Erasmus University
Digital Technologies for Public and Private Primary Care
- Design Thinking for Health Data Science Projects
- Patient Journey
- Clinical Pathway
- Data new vs old Wikipedia
- Findable
- Accessible
- Interoperable
- Reusable
- If we find a good solution, how do we scale? To another region, etc…
Jacson Venâncio Barros - President of the Brazilian Association of CIO’s in Health
Technologies for Supporting Public Health Management and Governance Problem: Startups are disconnected from end users
- 70% of hospitals don’t have eletronic medical records
- Lack of standards in vocabulary (taxonomy)
- Asymmetry of information: each specialty has its own jargon
- Lack of trust among health sectors Challenge: Identify in this sea of data, which is the drop that interests us
Round Table: Challenges of Big Data and AI in Population Health - Gisele Bohn, Richard Delaney, Nick Guldemond, Jacson Barros, Fatima Marinho
Topics:
- Aggregate behavioral data to clinical data
- Think small first: break problems into small questions that big data can help
- Predict events that are repeated in certain population groups
- Integration with the real world
- How social networks influence behaviour
Open Session: Data Access, Privacy and Security - Andrea Suman, Silvio Pereira, Anderson Soares, Marcelo Felix, Rogéria Leoni Cruz
- Restrictive law?
- Big Data x Data Governance
- No safe culture, territoriality, data sharing (would it restrict the access for research?)
- Loss of potential of using machine learning
Leonardo Rolim Ferraz
Data Driven ICU - Einstein Initiative
Lucas Bulgarelli - MIT/HIAE
Big Data 360
- MIMIC
- De-identification
- Leveraging electronic health records for clinical research
- Sharing - Physionet
Ary Serpa Neto - HIAE
Innovative Models of Clinical Trials Using Large Databases
Christopher Cosgriff - MIT
Deep Learning: A Brief Overview for Clinicians
Round Table: Challenges of Big Data and AI in the Intensive Care Unit - Leo Anthony Celi, Alistair Johnson, Leonardo Rolim Ferraz, Ary Serpa Neto, Lucas Bulgarelli
- The Book of Why
Leo Anthony Celi - MIT
MIT Experience in Data Analytics applied to Intensive Care Units
- MIMIC (Medical Information Mart for Intensive Care)
- Book: Secondary Analysis of Electronic Health Records
- Opportunities for AI in Healthcare
- Classification
- Prediction
- Optmization (Precision Medicine)
Alistair Johnson - MIT
Keynote: MIMIC Across Modalities: X-rays and Beyond
- Chest X-rays are ubiquitous, radiologists are not
- Perfect algorithms on imperfect reports
Matthieu Komorowski - Imperial College London
Keynote: Reinforcement Learning Approaches to Decision Support in Sepsis
Open Session: Opportunities for Innovation in Healthcare - Pedro Marton Pereira, Gustavo Landsberg, Gisele Bohn, André Bem
I forgot to take notes.
Datathon

Cauê Bueno, Eduardo Casaroto, Fernando Ramos, Gustavo Silveira, Jacqueline Silva,
Matheus Silva, Marcelo Fiorelli, Sonia Altavila, Wellington Araújo
Pulse Pressure: a new outcome predictor in the Intensive Care Unit?
Brief literature review and motivation for study
- Mean Arterial Pressure (MAP) is the main parameter used to define hemodynamic condition in critically ill patients and levels below 65mmHg are related to poor outcomes especially in septic patients
- Pulse Pressure (PP) is related to pressure and stroke volume.
- Pulse Pressure is a neglected hemodynamic parameter at bedside.
Aim of Study
Evaluate if Pulse Pressure is a reliable predictor of 28-days mortality compared to Mean Arterial Pressure in critically ill patients
Data Source
- Inclusion criteria:
- First ICU admissions (MIMIC-3)
- Exclusion criteria
- Patients readmitted at ICU in the same hospitalization
- Age < 18 years
Statistical analysis
- Description of the sample:
- mean and standard deviation
- bars plots and boxplots
- Logistic regression model
- Outcome: 28-days mortality (from ICU admission)
- Model 1: mean arterial pressure
- Model 2: pulse pressure
Results
Characteristis of the Sample
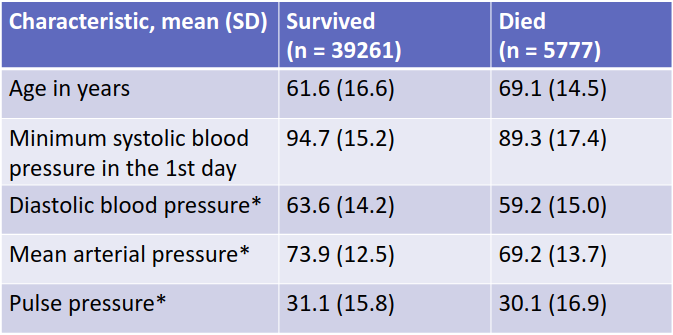
SD: standard deviation *Values taken when the minimum systolic blood pressure where observed in the first 24h of ICU admission
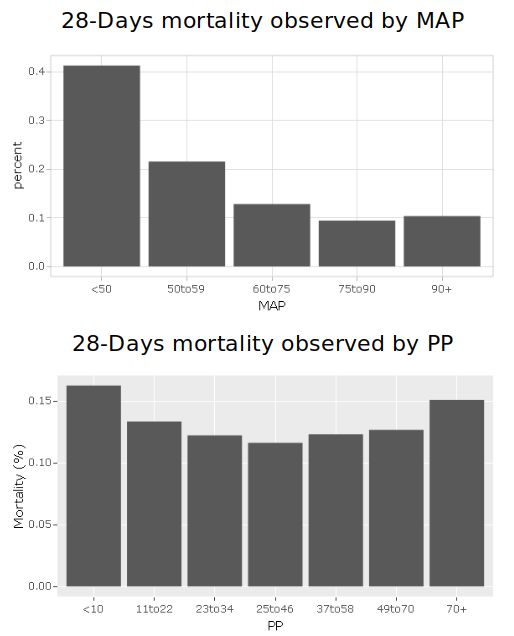
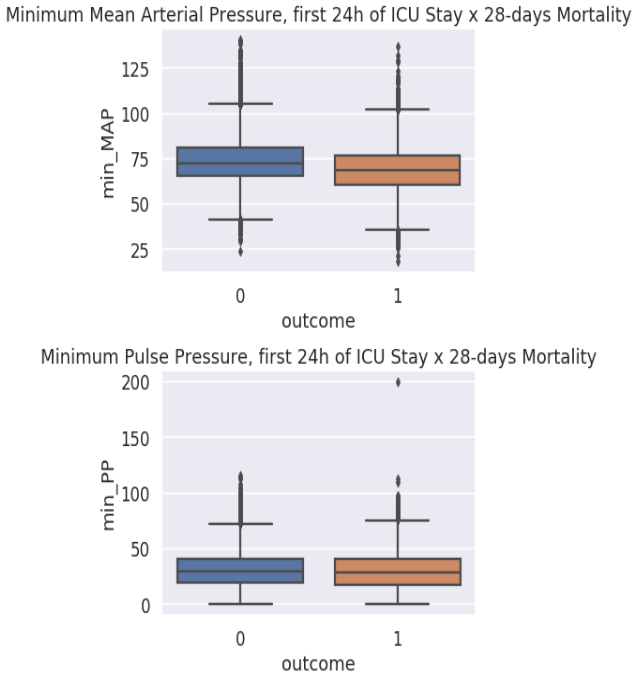
MAP vs PP
Logistic Regression
Outcome = 28-days mortality
Model 1: predictor = mean arterial pressure OR = 0.9694 95% IC = 0.9672 - 0.9717
Model 2: predictor = pulse pressure OR = 0.9960 95% IC = 0.9942 - 0.9977
Discussion and Next Steps
- MAP assessment alone might not be useful to predict outcome to all ICU patients
- Preliminary result: PP assessment looks to be a better outcome predictor for “higher PP” patients
- Promising results: min PP>70 - No min MAP difference between outcomes
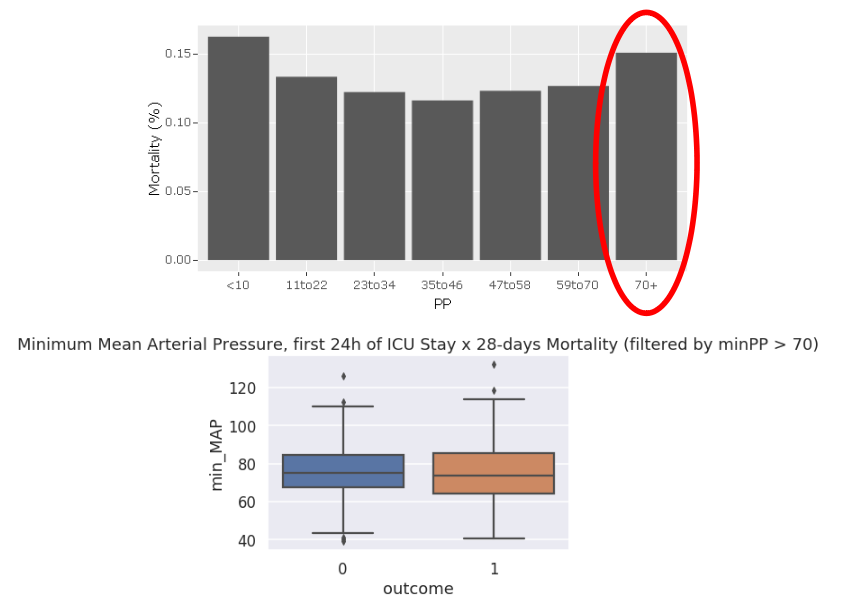
Next Steps:
- Group analysis: who are those patients? Are they elderly people?
- Check ICU interventions (mechanical ventilation, vasopressors etc)?
- Should we develop a specific guideline for those patients?